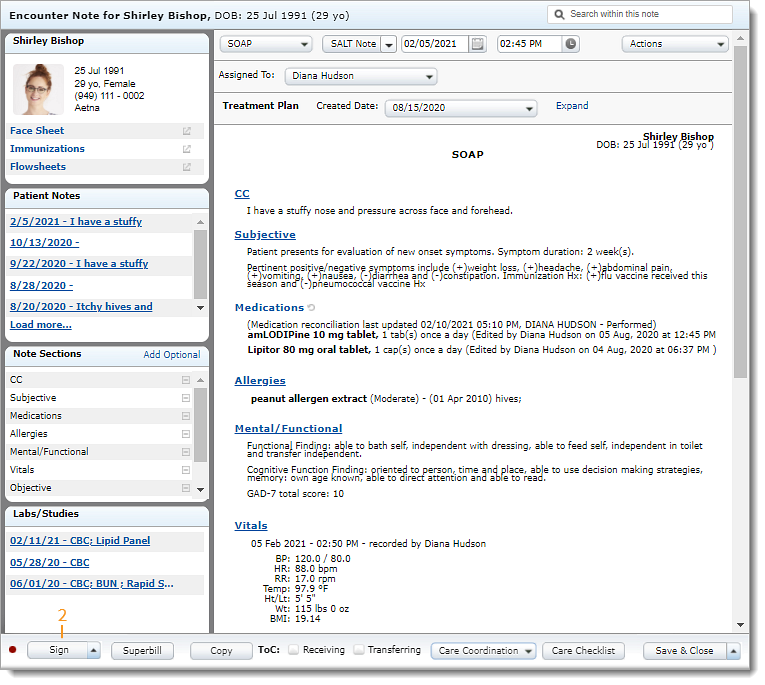
Sign Clinical Note
A note is the clinical documentation for a specific patient visit and can include problems, medications, allergies, immunizations, history, assessment, and treatment plan. Clinical notes can be edited until they are signed. Once the clinical documentation is completed, the provider signs the note to finalize the visit. If additional edit are required after the note is signed, add an addendum.
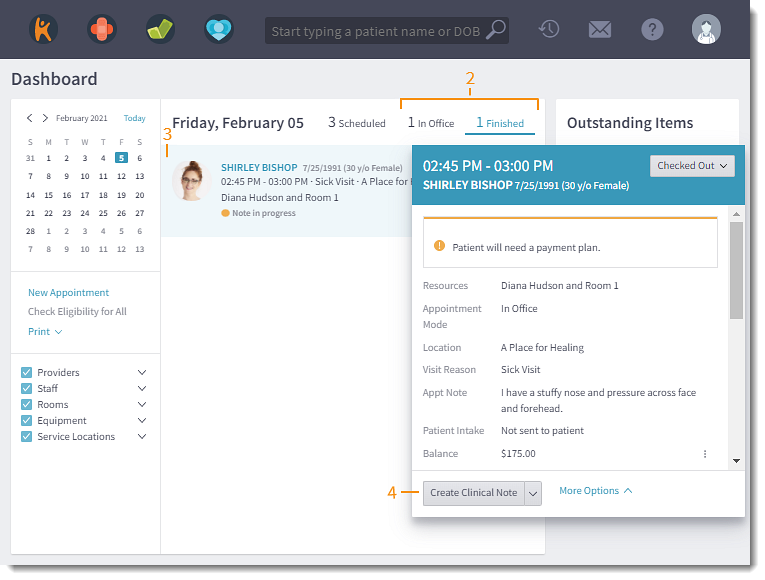
Open notes can be accessed from various locations: the patient's appointment on the Dashboard, Open Notes, or the patient's Notes tab.
Access Clinical Note
|
 |
Sign Clinical Note
|
 |