Add 12 Diagnosis Codes to a Claim
Some payers recognize the need to include more than four unique diagnosis codes for a procedure on a claim and provide alternate reporting methods. There are two available workflows to accommodate this need. Each procedure code on the encounter can have a maximum of four diagnosis codes, so the first workflow allows the submission of up to eight additional diagnosis codes with that procedure code and four primary diagnosis codes. The second workflow adds two additional service lines to submit with that procedure code and divides up to 12 diagnosis codes between the three lines of service.
Note: These solutions may not be accepted by all payers. Contact the payer directly to verify their specific requirements for submitting 12 diagnosis codes then proceed with the appropriate workflow.
To submit up to 12 diagnosis codes:
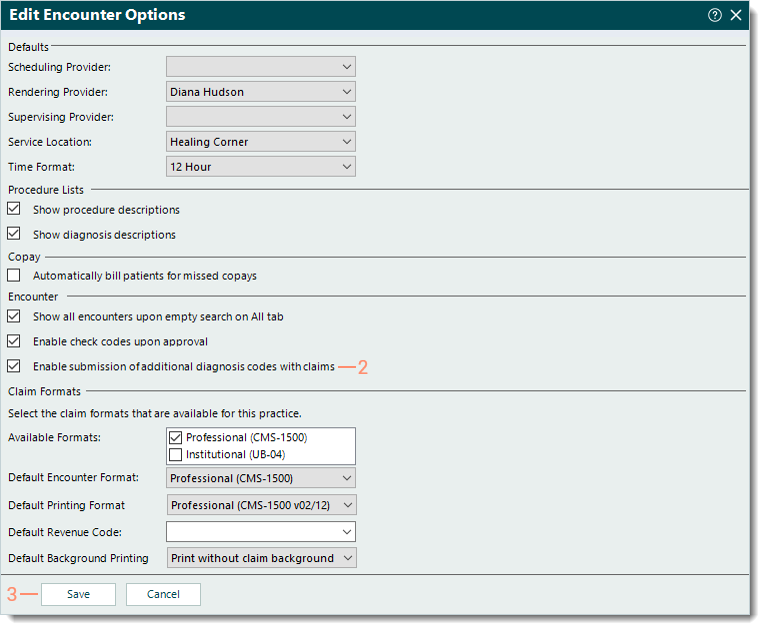
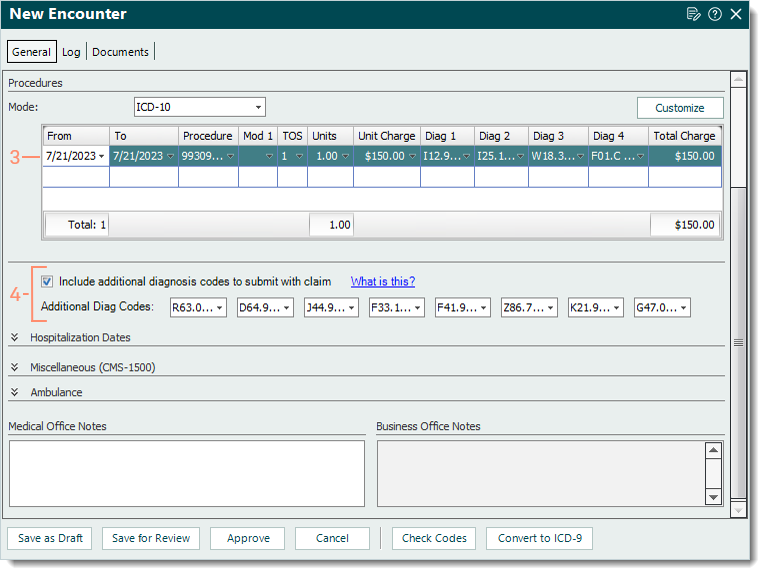
- For a single procedure code, a System Administrator must first enable the encounter option that allows the submission of additional diagnosis codes with claims. Once enabled, the option to include additional diagnosis codes displays on the encounter. When creating the encounter, click to select this option then enter the additional diagnosis codes in the available fields.
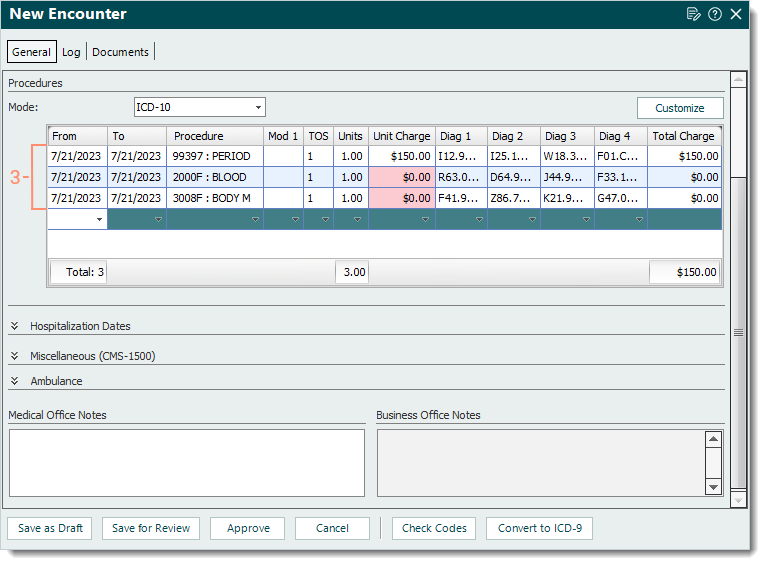
- By adding two more lines of service, create the encounter and divide the 12 diagnosis codes between the three lines of service. Service line 1 has the main procedure code and four primary diagnosis codes. Service lines 2 and 3 have additional services performed during the patient visit (e.g., BMI or blood pressure) and the remaining eight diagnosis codes.
Note: The two additional procedure codes must be relevant to the patient visit, but they do not need to be associated with the diagnosis codes.
Enable Option to Submit Additional Diagnosis CodesSystem Administrators can enable the encounter option to submit additional diagnosis codes with claims when necessary. Once enabled, the "Include additional diagnosis codes to submit with claim" option becomes available on the Encounter record.
|
 |
Enter Additional Diagnosis Codes on EncounterOnce the encounter option to submit additional diagnosis codes has been enabled, follow the steps below to create the encounter and enter the additional codes.
|
 |
Enter Additional Service Lines and Diagnosis CodesFollow the steps below to add two additional service lines to submit with the main procedure code and divide up to 12 diagnosis codes between the three lines of service.
|
 |