Your claims cannot be submitted to the secondary insurance because the charge amount does not equal the sum of the paid amount and all line adjustment amounts
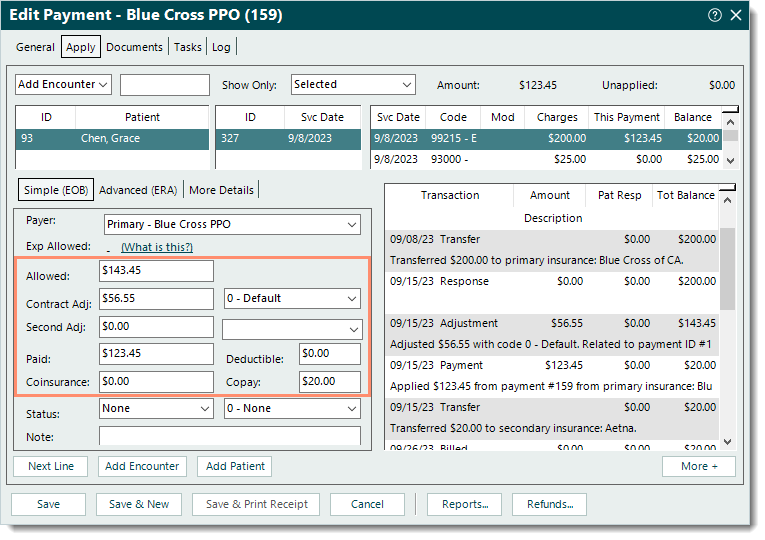
Rejection MessageYour claims cannot be submitted to the secondary insurance because the charge amount does not equal the sum of the paid amount and all line adjustment amounts. This would result in a rejection at the clearinghouse. Please open Encounters > Track Claim Status, then find the claim ID above, review the transaction history, locate and open the payment from the primary insurance, and finally, review the amount paid by the primary and all line adjustments amounts and make any necessary corrections. The primary paid amount + all line adjustments must equal the original service line charge. |
|
Rejection DetailsTebra Validation Error This rejection indicates the sum of the paid amount and all line adjustment amounts do not equal to the charge amount for the primary payment. Claims billed with an invalid paid and adjustment amount will reject at the clearinghouse; therefore Tebra has held the claim until the error is corrected. Once the error is corrected, resubmit the claims in order for them to be sent to the clearinghouse. Note: Since claims rejected within Tebra are not forwarded to the clearinghouse, timely filing cannot be generated for the submission until the validation errors have been corrected and the claims are successfully submitted to the clearinghouse. |
|
ResolutionFollow the steps below to correct the posted payment:
Then, rebill and resubmit all affected claims when ready. |
 |