Missing other payer subscriber's insurance policy number, plan name:
|
Rejection Message Missing other payer subscriber's insurance policy number, plan name: |
|
|
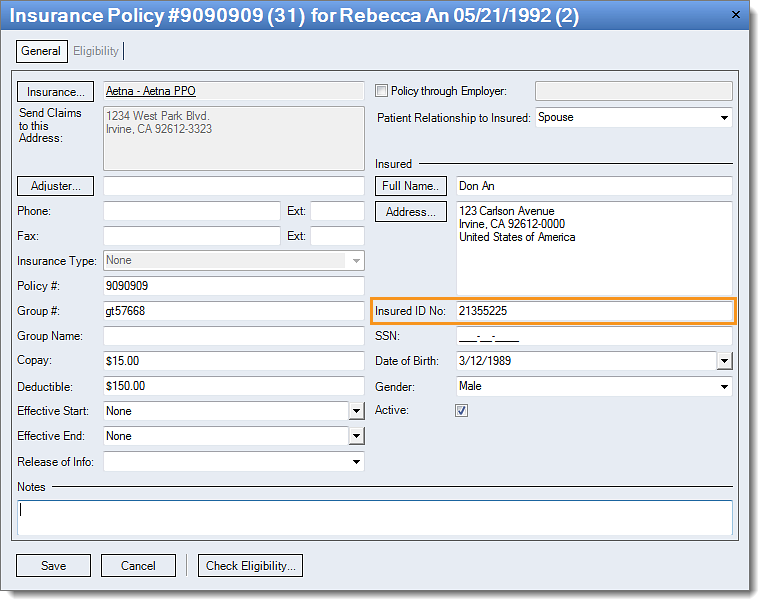
Rejection Details Kareo Validation Error This rejection indicates the patient’s insurance policy is through another individual but a policy number has not been populated for the Insured. Claims billed without a policy number for the Insured will reject at the clearinghouse; therefore Kareo has held the claim until the error has been corrected. You must correct the error and resubmit the claims in order for them to be delivered to the payer. Note: Since claims rejected within Kareo are not forwarded to the clearinghouse you will be unable to generate timely filing for that submission until validation errors have been corrected and the claim resubmitted. |
|
|
Resolution Follow the instructions below enter the policy number for the insured:
Then, rebill and resubmit all affected claims. |
 |
| Tip: Most subscription levels include access to a free eligibility check feature which can be used with many payers to verify a patient has active coverage. Utilizing this feature prior to submitting claims for a patient can help prevent this type of rejection. | |