5010 Edit: Procedure code XXXXX is an NOC type code and requires a description note per service line
Rejection Message5010 Edit: Procedure code [XXXXX] is an NOC type code and requires a description note per service line. |
|
Rejection DetailsTebra Validation Error This rejection indicates the claim contains a Not Otherwise Classified (NOC) code that requires a detailed text description. Claims billed without a description for a NOC code will reject at the clearinghouse; therefore Tebra has held the claim until the error is corrected. Once the error is corrected, resubmit the claims in order for them to be sent to the clearinghouse. |
|
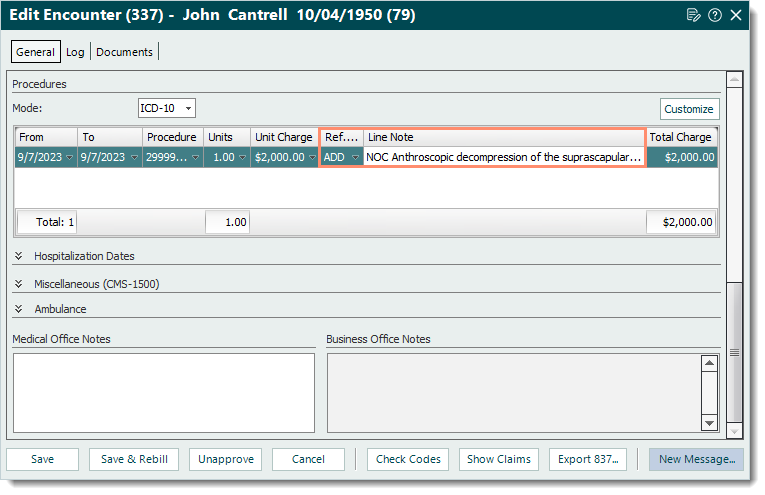
ResolutionFollow the steps below to enter an NOC code description:
Then, resubmit all affected claims when ready. |
 |