- If a corrected claim needs to be resubmitted with a specific claim frequency code, follow the instructions below to enter the Submit Reason in the encounter.
Note: When unsure, contact the payer and verify the required information to prevent further claim rejections and processing delays. For example, Medicare does not accept any claim frequency code other than 1 to indicate the claim is an original claim.
- Click Encounters > Track Claim Status. The Find Claim window opens.
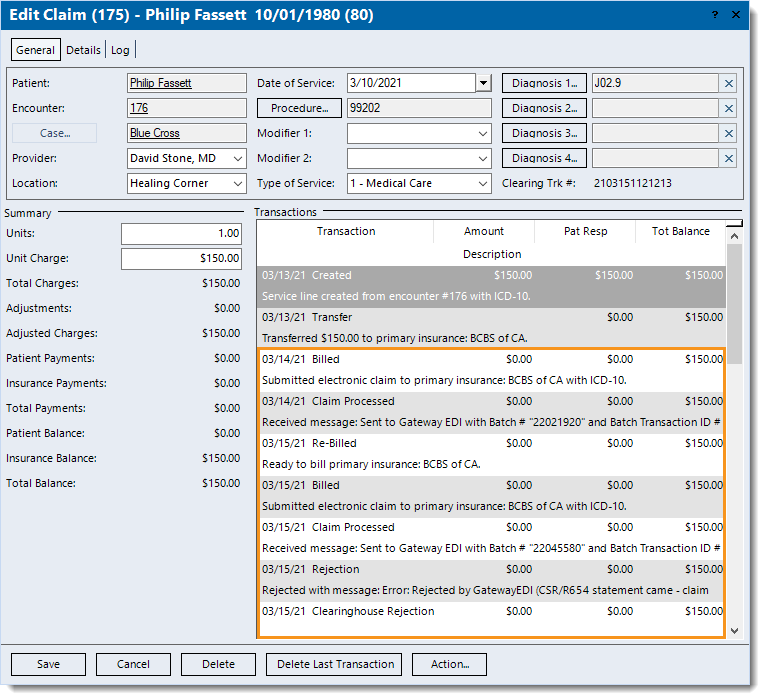
- Find and double click the claim that needs correcting. The Edit Claim window opens.
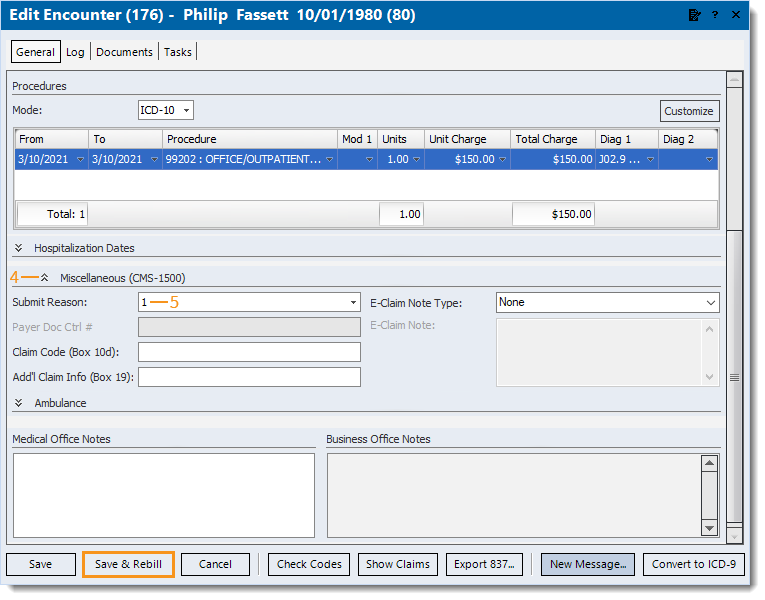
- Double click on the Encounter ID number. The Edit Encounter window opens.
- Click the double arrow to expand the Miscellaneous section.
- Click to select the payer required Submit Reason code.
- If Submit Reason code 6, 7, or 8 is selected, enter the associated Payer Doc Ctrl # (Payer Document/Claim Control Number) as required by the payer for claim processing.
- If the payer requires the Submit Reason to appear in other areas of the claim, follow the below steps.
- For paper claims, enter the information as follows:
- Claim Code (Box 10d): Enter up to 19 characters to report appropriate claim codes to identify additional information about the claim.
- Add'l Claim Info (Box 19): Enter up to 71 characters to identify additional information about the claim.
- For e-claims, click the E-Claim Note Type drop-down arrow and select Additional Information. Then, enter the required information as an E-Claim Note.
- Click Save & Rebill. Then, resubmit all affected claims once all corrective actions are complete.
|
 |