Requests for readjudication must reference the newly assigned payer claim control number
|
Rejection Message Requests for readjudication must reference the newly assigned payer claim control number. |
|
|
Rejection Details This rejection indicates an incorrect Payer Claim Control number was submitted on the claim. |
|
|
Resolution Please use the original claim control number for the first submission. If necessary, the submitter can call the payer to obtain this information. |
|
|
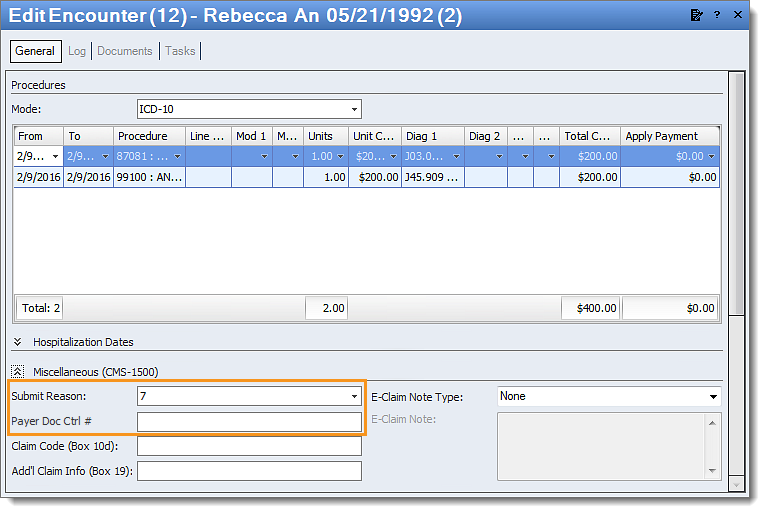
Follow the instructions below to enter the correct payer claim control number on the encounter:
Then, resubmit all affected claims. |
 |