Rejected for Invalid Information NDC Number
Views: 14891
Rejection MessageREJECTED FOR INVALID INFORMATION NDC NUMBER. NDC NUMBER. NDC NUMBER |
|
Rejection DetailsThis rejection indicates the claim includes a procedure (CPT/HCPCS) code with an invalid National Drug Code (NDC) number. |
|
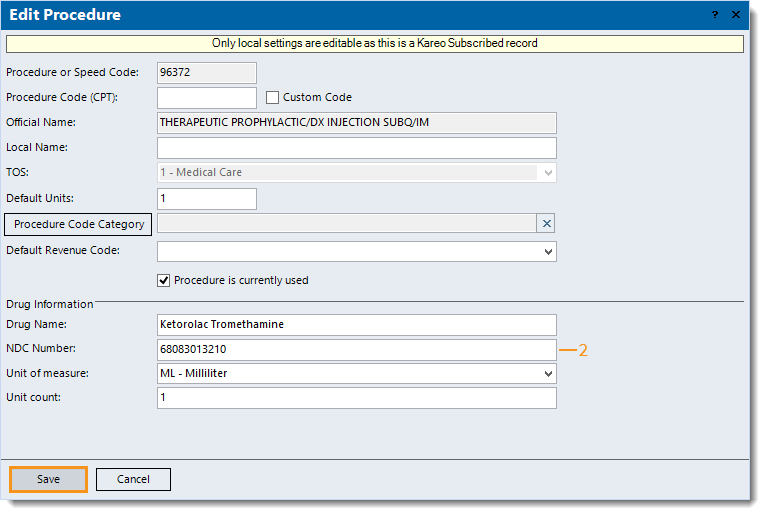
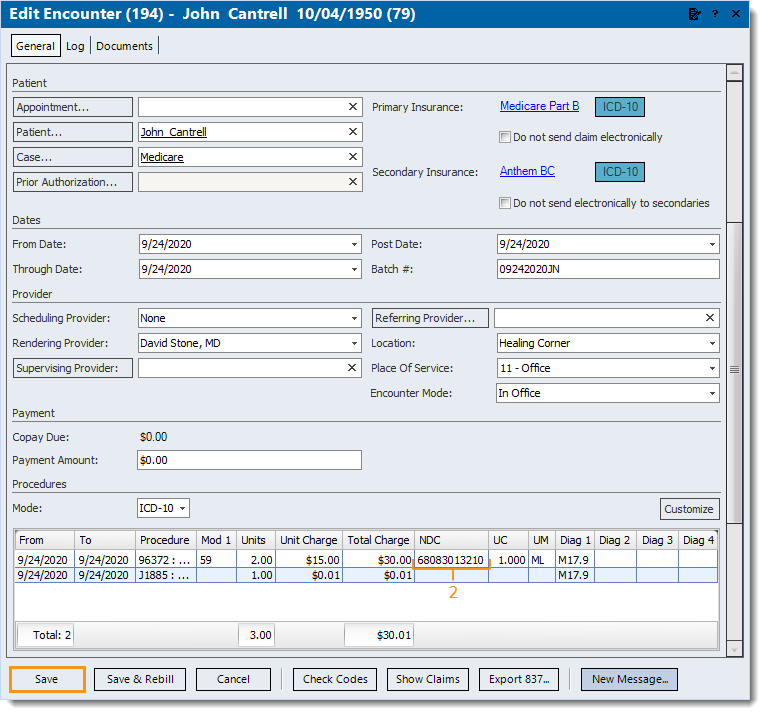
ResolutionFollow the steps below depending on whether the National Drug Code (NDC) number was entered in the Procedure or Encounter record.
Then, rebill and resubmit all affected claims. |
|
Then, rebill and resubmit all affected claims. |
 |