Procedure Code Modifier(s) for Service(s) Rendered Acknowledgement/Rejected for Invalid Information
|
Rejection Message Procedure Code Modifier(s) for Service(s) Rendered Acknowledgement/Rejected for Invalid Information |
|
|
Rejection Details This rejection indicates (per the payer) one of the procedure (CPT/HCPCS) modifiers submitted on the claim was invalid for the date of service being billed. |
|
|
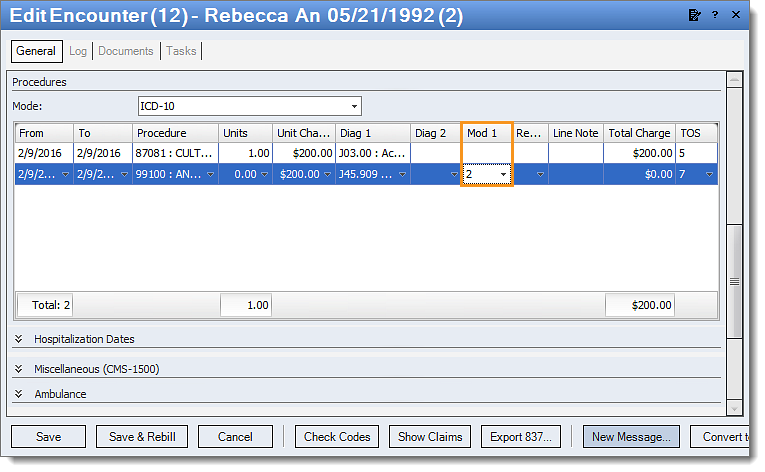
Resolution Follow the instructions below to edit the modifiers included on an encounter:
Then, resubmit all affected claims. |
|
|
Tip: Most subscription levels include access to a free code scrubbing tool on the Encounter. Utilizing this feature for all encounters can help prevent code rejections. Note: Kareo Support cannot provide coding assistance. Please contact your biller/coder with any CPT or ICD code questions. |
|