|
Rejection Message
Other Payer Insurance Type is required when Payer is Medicare (Not Primary)
|
|
Rejection Details
This rejection has two possible causes:
- Medicare is listed as secondary insurance on the patient's case and the Insurance Type field on the policy page has been left blank.
- Both insurances billed on the claim was Medicare. When Medicare is listed as one of the payers on a claim, the other payer(s) listed cannot also have an Insurance Program of MB- Medicare Part B.
|
|
Resolution
Resolution steps will vary depending on the cause.
|
|
|
If Medicare is the secondary, follow the instructions below to enter the insurance type code:
- Click Encounters > Track Claim Status. The Find Claim window opens.
- Look for and double-click on the encounter that needs correcting. The Edit Claim window opens.
- Double-click on the Case. The Edit Case window opens.
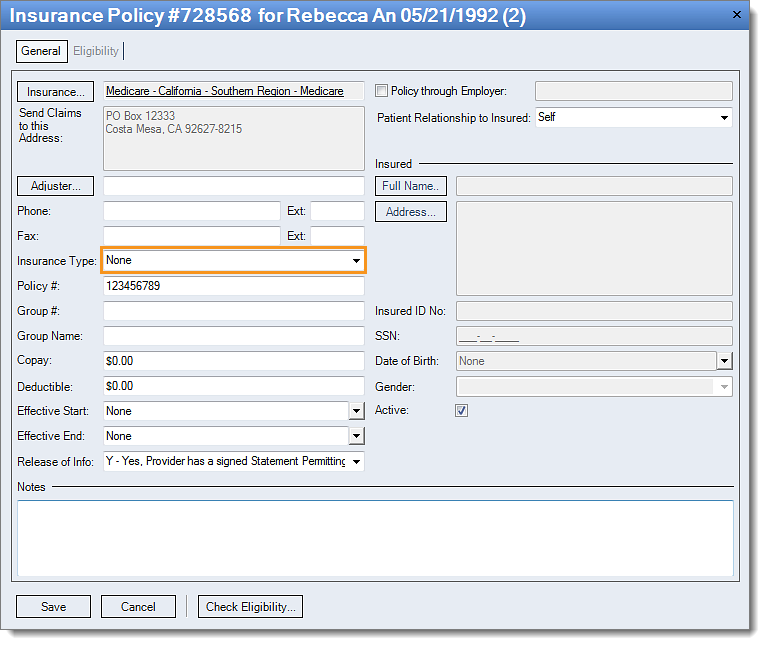
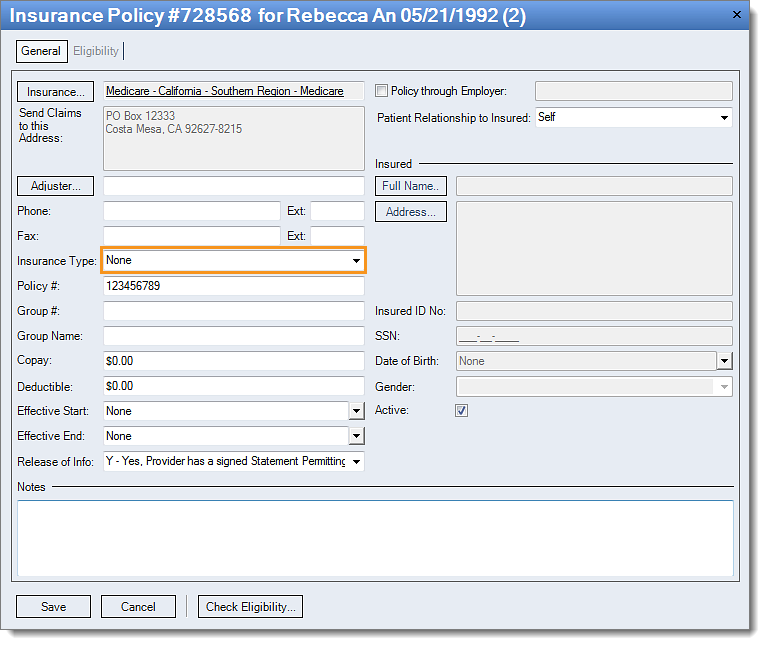
- Double-click on the Medicare policy listed as secondary. The Insurance Policy window opens.
- Select the correct Insurance Type from the drop-down menu.
- Click Save all the way out (multiple saves may be required).
Then, rebill and resubmit all affected claims.
|
 |
|
If the insurance program was incorrectly setup, follow the instructions below to change the insurance program code:
- Click Encounters > Track Claim Status. The Find Claim window opens.
- Look for and double-click on the encounter that needs correcting. The Edit Claim window opens.
- Double-click on the Case. The Edit Case window opens.
- Double-click on the appropriate Insurance Policy. The Insurance Policy window opens.
- Double-click on the Insurance Name. The Edit Insurance Plan window opens.
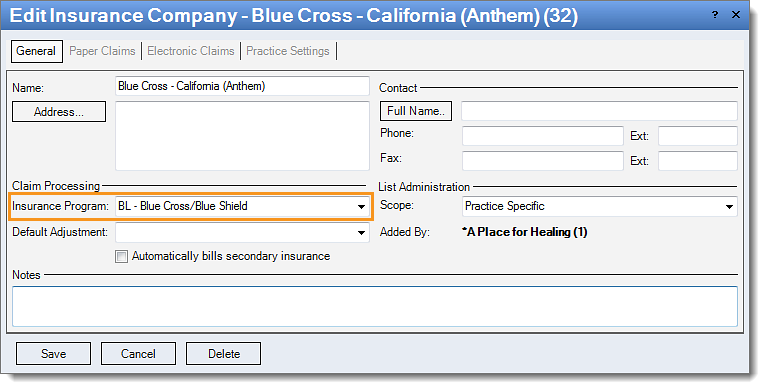
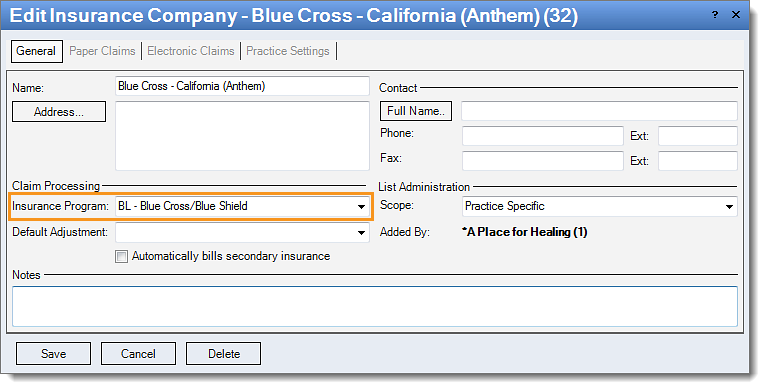
- Double-click on the Insurance Company
name. The Edit Insurance Company window opens.
- Click the Insurance Program drop-down to select the correct insurance program code.
- Click Save all the way out (multiple saves may be required).
Then, rebill and resubmit all affected claims.
|
 |