Ordering provider required for DMERC claims
|
Rejection Message Ordering provider required for DMERC claims |
|
|
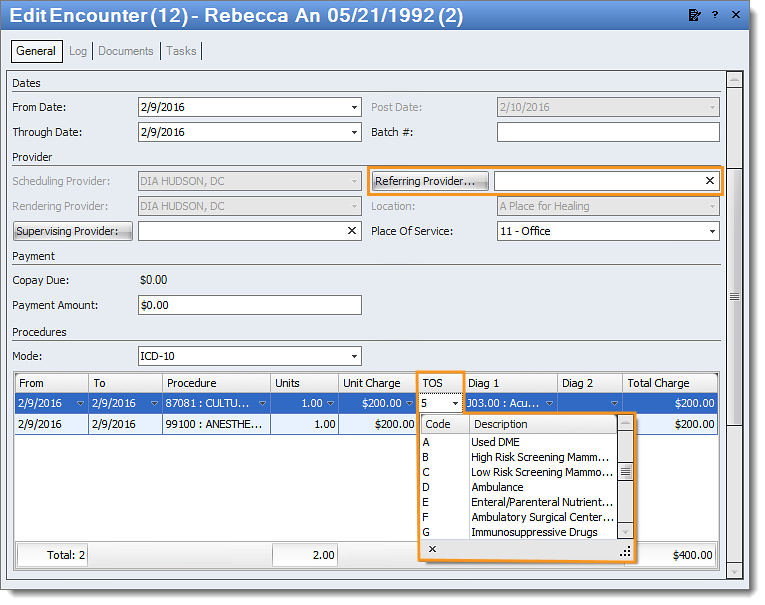
Rejection Details This rejection indicates the ordering provider is required. In Kareo, the ordering provider is pulled from the Referring Provider field and will populate when the Type of Service (TOS) is a DME code. |
|
|
Resolution Follow the instructions below to add the Ordering Provider to the encounter:
Then, resubmit all affected claims. |
 |