Claim Level Date is Missing or Invalid. Date Must be in the CCYYMMDD Format - CMS-1500
|
Rejection Message Claim Level Date is Missing or Invalid. Date Must be in the CCYYMMDD Format Note: Several rejections will include this wording. If the rejection message also includes "RELATED CAUSE INFORMATION IS MISSING OR INVALID," the cause and resolution steps will be different than those outlined in this entry. Please see the corresponding entry for that rejection for further information. |
|
|
Rejection Details This rejection occurs for both professional and institutional claims and indicates that the Admission Date/Hour was sent out on the claim, but should not have been. It may be used only on inpatient claims (and some outpatient claims) as defined by the NUBC (National Uniform Billing Committee). Segment DTP (Admission Date/Hour) has been populated onto the encounter. Segment DTP is defined in the guideline at position 1350 of the ANSI 837I (institutional) and loop 2300 DTP*435 of the ANSI 837P professional) EDI file. |
|
|
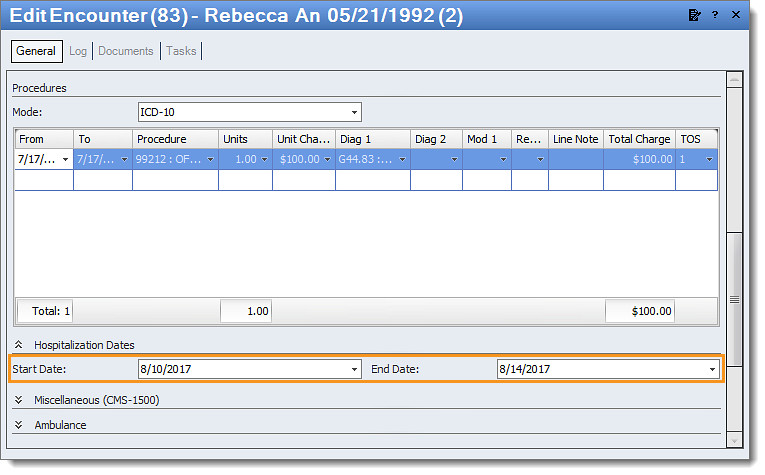
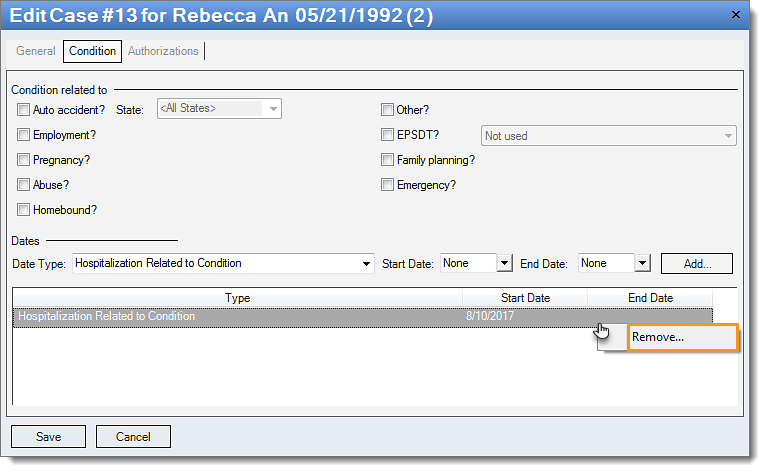
Resolution The hospitalization dates will need to be removed from the claim. There are two places where the date may have been entered. Follow the appropriate steps below to remove the date. |
|
|
Follow the instructions below to remove the hospitalization dates on the encounter:
Then, resubmit all affected claims. |
 |
|
Follow the instructions below to remove the hospitalization date from the patient case:
Then, rebill and resubmit all affected claims. |
 |