Claim Frequency Code Acknowledgement/Rejected for Invalid Information
|
Rejection Message Claim Frequency Code Acknowledgement/Rejected for Invalid Information |
|
|
Rejection Details This rejection indicates that an incorrect submission reason was included on the claim per the payer’s requirements. The “Invalid Claim Frequency Code” refers to the Submit Reason selected on the encounter. The appropriate submission code depends on the payer’s requirements. For example, most Medicare payers will not accept any claim submission reason other than “1 –Original.” |
|
|
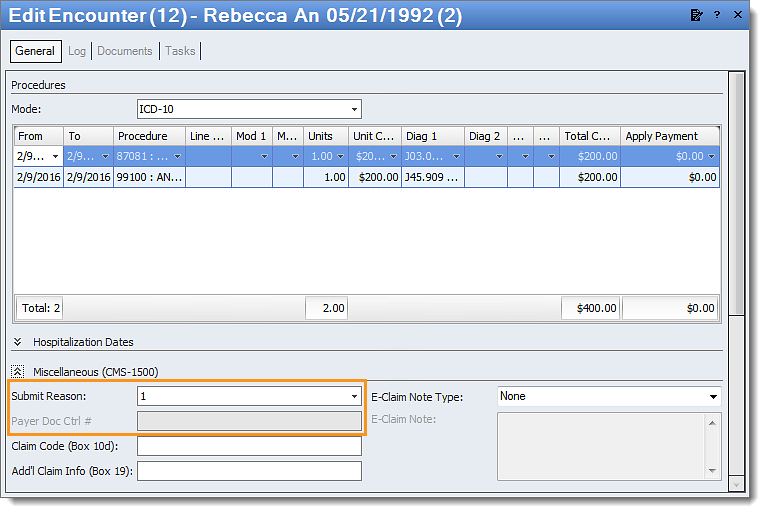
Resolution Follow the instructions below to enter the submit reason on the encounter:
Then, resubmit all affected claims. |
|