Rejection Message
Adjudication or Payment Date is required when sending Line Adjudication Information. 2430.DTP*573
|
Rejection Details
This rejection indicates the adjudication date is missing on the payment from the primary payer.
|
Resolution
Follow the steps below to add an Adjudication Date to the primary payment and to also verify the primary payer's Practice Settings is configured to send coordination of benefits (COB) information:
- Click Encounters > Track Claim Status. The Find Claim window opens.
- Look for and double click the appropriate claim to open. The Edit Claim window opens.
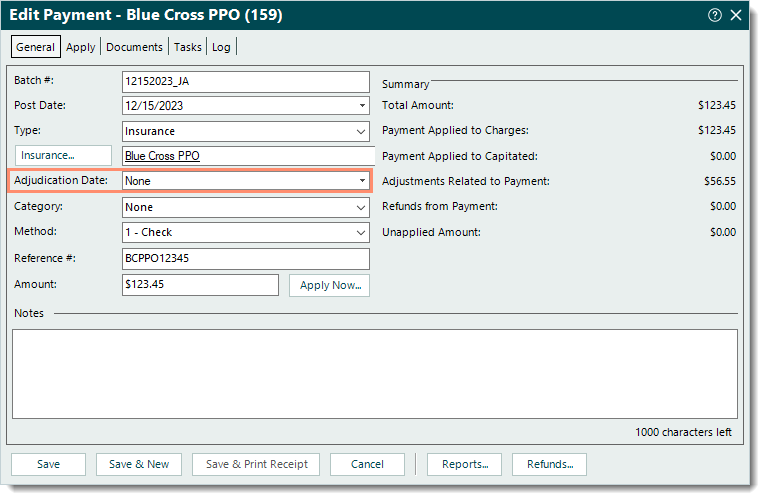
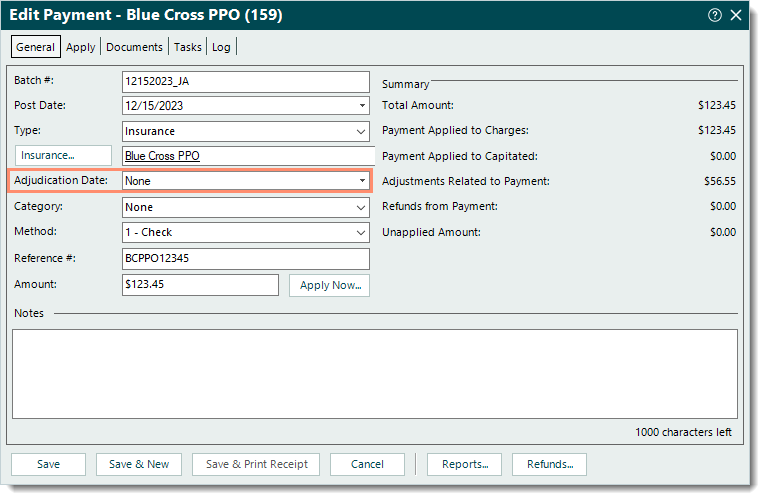
- Under the Transactions section, double click the primary Payment transaction line. The Edit Payment window opens.
- Enter the Adjudication Date for the payment.
- Click Save. The Edit Claim window returns.
|
 |
- Double click the Case name. The Edit Case window opens.
- Double click the appropriate policy listed as the primary payer. The Insurance Policy window opens.
- Double click the Insurance name. The Edit Insurance Plan window opens.
- Double click the Insurance Company name. The Edit Insurance Company window opens.
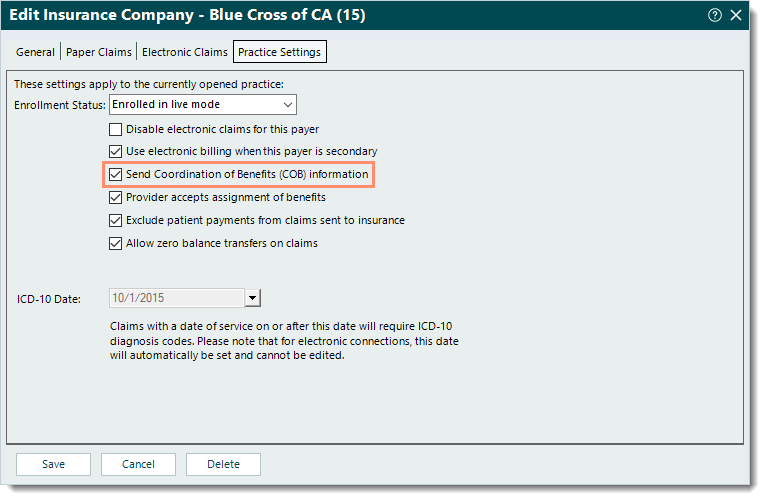
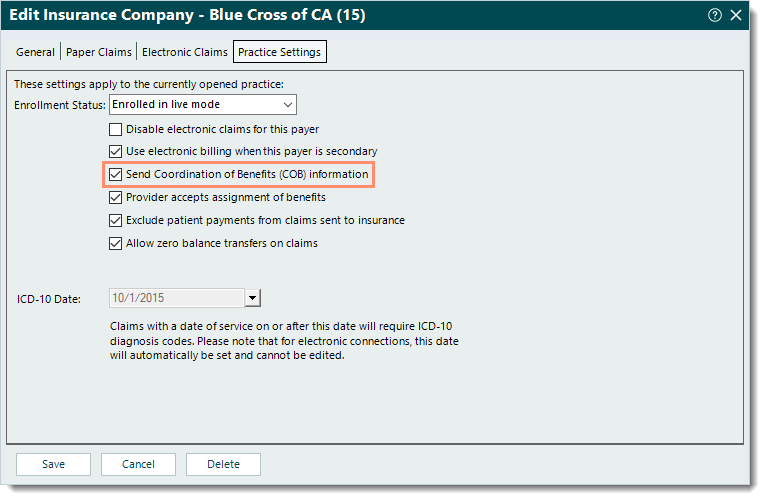
- Click the Practice Settings tab. The practice settings information displays.
- If necessary, click to select "Send Coordination of Benefits (COB) information".
- To save any changes made, click Save at the bottom of each relevant insurance window until it is no longer available.
Then, rebill and resubmit all affected claims when ready.
|
 |