|
Rejection Message
ACKNOWLEDGEMENT/RETURNED AS UNPROCESSABLE CLAIM THE CLAIM/ENCOUNTER HAS BEEN REJECTED AND H
|
|
Rejection Details
This rejection message and solution is specifically for claims billed to Humana.
The actual rejection in their system is: DUPLICATE OF A PREVIOUSLY PROCESSED CLAIM/LINE
This rejection message indicates that the payer has received the exact claim or service before. This rejection has two possible causes:
- The exact claim was resubmitted within 48 hours of the last submission.
- The submission reason code and additional information was not included on the corrected claim that was resubmitted.
|
|
Resolution
Resolution steps will vary depending on the cause:
|
- If the exact claim was submitted within 48 hours of the previous claim, contact the payer to verify the status of the previous claim submission. Determine if the claim needs to be corrected and (if so) how to properly resubmit.
- If the initial claim is still processing, this rejection will not affect the status of the initial submission.
|
|
- If the claim needs to be resubmitted as a corrected claim (per payer request), follow the instructions below to enter the submit reason on the encounter:
Note: The submit reason code depends on the payer's requirements. For example, Medicare will not accept any Claim Submission Reason Code other than “1 –Original.” Do not change the Submit Reason unless you are certain the payer needs it changed.
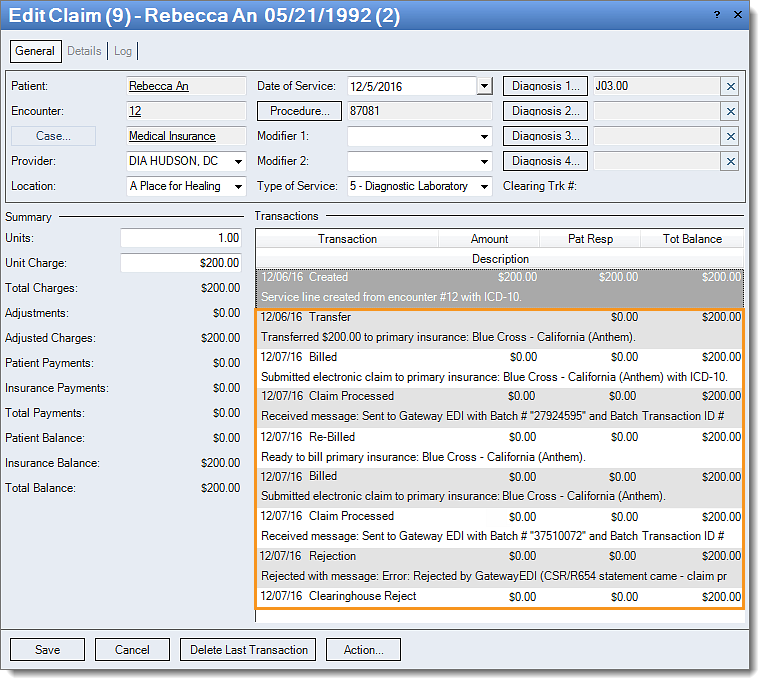
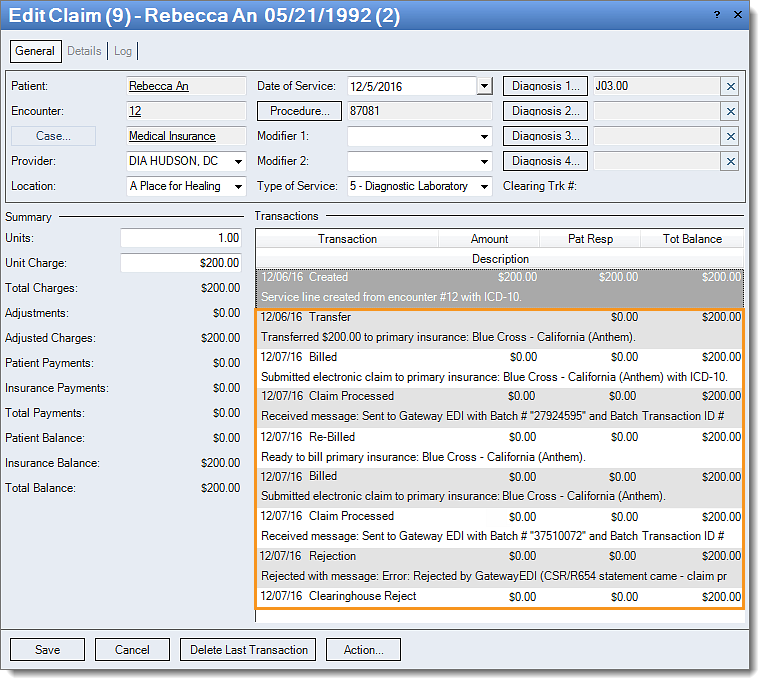
- Click Encounters > Track Claim Status. The Find Claim window opens.
- Look for and double-click on the encounter that needs correcting. The Edit Case window opens.
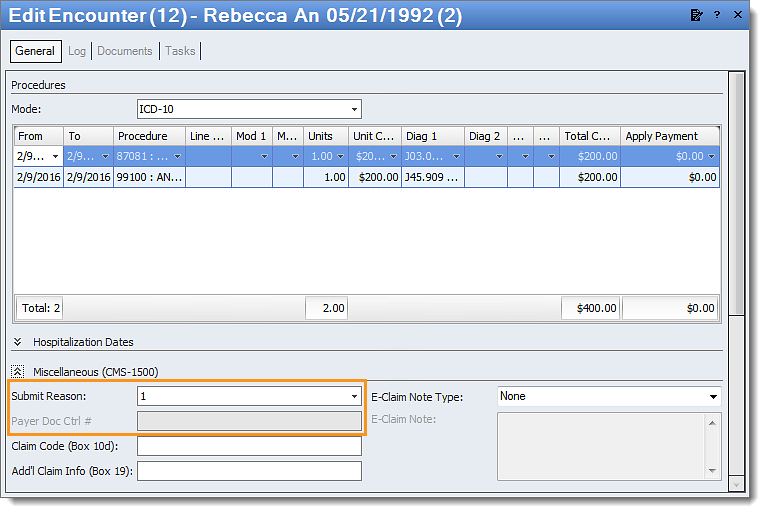
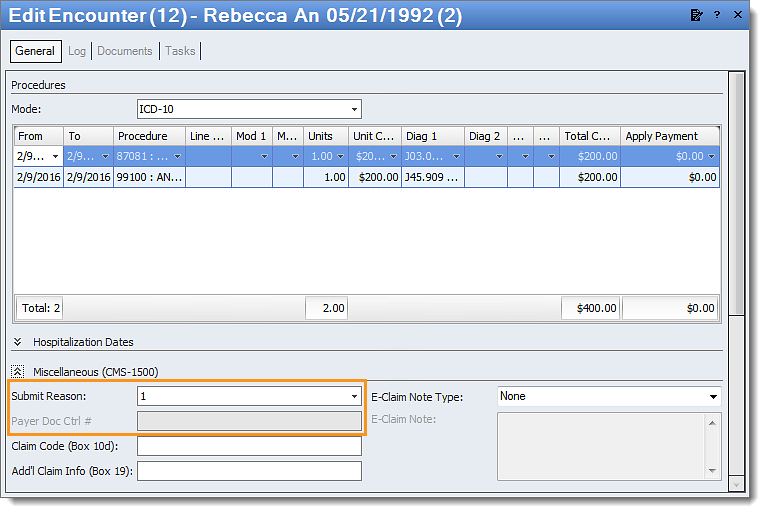
- Double-click on the Encounter number. The Edit Encounter window opens.
- Click the arrows next to Miscellaneous to expand.
- Select the correct Submit Reason code. The Submit Reason code depends on the payer’s requirements. Contact the payer directly with any questions about correct claim submissions.
- Enter the Payer Doc Ctrl # (if the field is not grayed out).
- The payer may require the Submit Reason to appear in other areas of the claim.
- On Paper: Enter information in the appropriate field – either box 10D or 19.
- Electronically: Write the Submit Reason as an e-claim by selecting "Additional Information" in the e-Claim Note Type.
- Click Save & Rebill.
Then, resubmit all affected claims.
|
 |