Insurance Company Practice Settings
- Last updated
-
-
Save as PDF
Updated: 11/30/2023 | Views: 7921
The Practice Settings of the insurance company allows you to select paper and electronic claims (e-claims) billing settings specific to the currently open practice and does not affect other practices (when there are multiple) within the Tebra account.
Note: To set the enrollment status of electronic claims billing for the entire practice, go to the Electronic Claims Options.
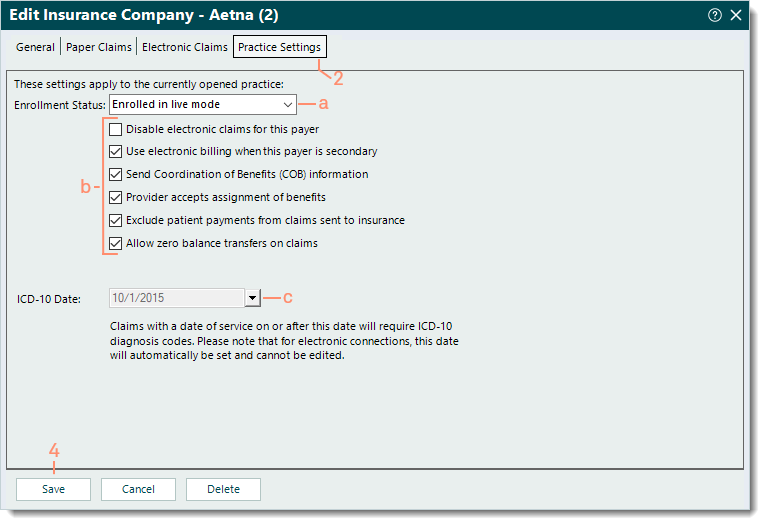
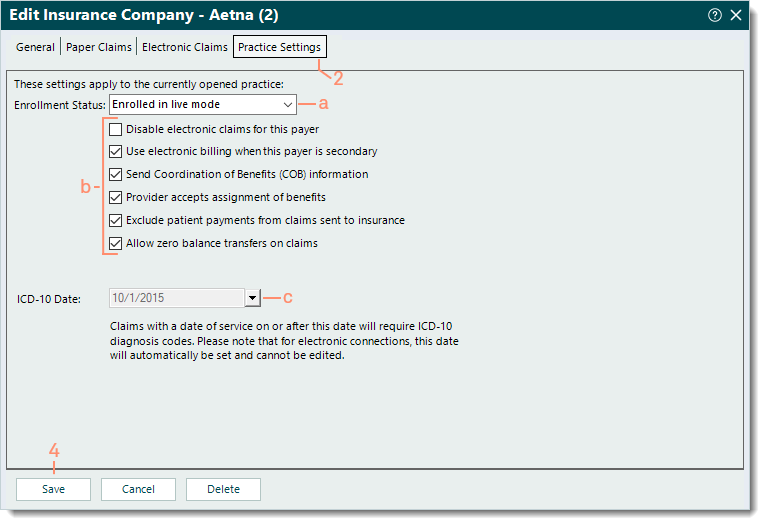
Configure Practice Settings
- Find the insurance company then click the insurance name to open. The Edit Insurance Company window opens.
- Click the Practice Settings tab. The Practice Settings information displays.
- Select the appropriate practice settings for the insurance company.
- Enrollment Status: Click the drop-down arrow to select a status.
- Enrolled in live mode: Select this status to allow e-claims submission once this payer's Claims status shows as Approved on the Enrollments Dashboard.
- Not enrolled (default) and all other statuses prevent e-claims submission to this payer.
- Click to select or clear the selected options as necessary:
- "Disable electronic claims for this payer" prevents e-claims submission to this payer.
- "Use electronic billing when this payer is secondary" allows secondary e-claims submission to this payer.
- "Send Coordination of Benefits (COB) information" includes the COB information on secondary claims.
- "Provider accepts assignment of benefits" populates Box 27 of the CMS-1500 paper claim form and Loop 2300 CLM08 for e-claims.
- "Exclude patient payments from claims sent to insurance" bills the total charge amount to the payer even if patient payments were applied. This option populates Box 29 of the CMS-1500 paper claim form and Loop 2300 AMT02 for e-claims with $0.00.
- "Allow zero balance transfers on claims" transfers all line items of the claim including those with zero balances.
- ICD-10 Date: The payer's conversion date to ICD-10 coding.
- If the payer is set up as a commercial payer, the date is shaded and cannot be changed.
- Click Save to record any changes.
|
 |