Enrollment Status Indicators
After submitting enrollment requests for electronic insurance service(s) for Claims, Eligibility and/or ERAs, refer to the Enrollments Dashboard for status updates and items that require action from the practice.
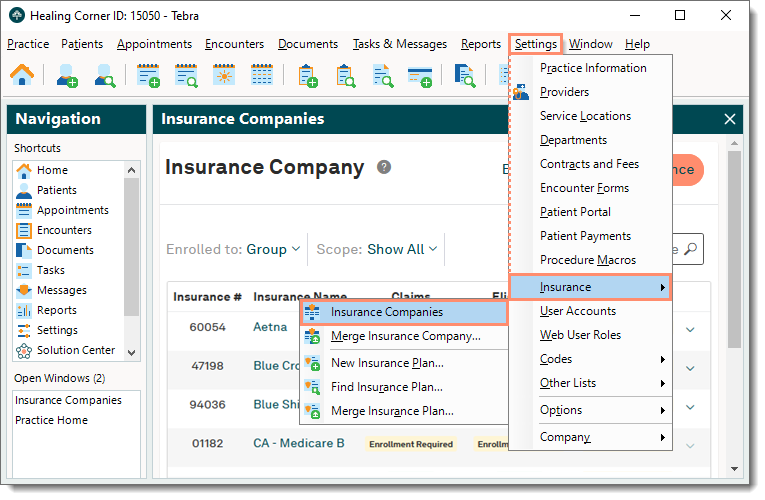
Navigate to Enrollments Dashboard
|
 |
Enrollment Status Indicators
| Status | Description | Displays When | Next Step |
| Approved | Claims: Start sending claims immediately. Eligibility: Start checking eligibility immediately. ERAs: Does not apply. |
The payer has either approved the enrollment request or enrollment is not required. | Configure settings for each insurance company. |
| Request Received | The enrollment request has been received by Tebra. | The enrollment request has been submitted but not yet triaged. | No action required by the practice. |
| Work in Progress | The enrollment request is under review by the Tebra Enrollments. | The enrollment request is being triaged. | Tebra Enrollments prepares forms for payer enrollment. Note: If additional information is required, emails are sent to the contact provided in step 5 of Enrollments wizard. |
| Pending Insurance | The request has been sent to the payer for processing. | All payer enrollment forms have been submitted to the payer. | Tebra Enrollments follows up with the payer for enrollment processing updates. |
| Pending First ERA | Claims: Does not apply. Eligibility: Does not apply. ERAs: Pending first ERA from the payer. Please allow 30-45 days for delivery. |
The enrollment has been approved by the payer and the practice is waiting for an ERA to be received in the Desktop Application (PM). | Once the ERA is received in the Desktop Application (PM), post the payment. |
| ERA Received | Claims: Does not apply. Eligibility: Does not apply. ERAs: Enrollment request is approved and the practice is receiving ERAs. |
At least one ERA has been received from the payer and the payment has been posted in the Desktop Application (PM). | No further action required. |
| Action Required | Enrollment cannot continue until action items are resolved by the practice. | Action is required by the practice to complete enrollment. | Check email for enrollment instructions. Note: Emails are sent to the contact provided in step 5 of Enrollments wizard. |
| N/A | Claims: The payer does not support electronic claims. Eligibility: The payer does not support electronic eligibility checks. ERAs: The payer does not support ERAs. |
The electronic service is not supported by the payer, clearinghouse, or Tebra. | No further action required. |
| Cancelled | The enrollment request has been canceled. | The enrollment request has been canceled. Reasons for cancelation may include: customer request, duplicate submission, or the payer is no longer active. | If necessary, submit a new enrollment request for the payer. Otherwise, no further action required. |
| Denied | The enrollment request has been denied by the payer. | The enrollment request has been denied by the payer. | Check email for information about the enrollment denial. Note: Emails are sent to the contact provided in step 5 of Enrollments wizard. |
| On Hold | The enrollment request is on hold. Please check email for details. | Enrollment cannot continue for an undetermined length of time due to a processing issue with the payer, clearinghouse, or Tebra. | Check email for additional information. Note: Emails are sent to the contact provided in step 5 of Enrollments wizard. |
| Expired | The practice did not complete action items and the enrollment request has expired. | The action items have not been completed within 45 business days. | Check email for information. To continue enrollment, submit a new enrollment request for the payer. Note: Emails are sent to the contact provided in step 5 of Enrollments wizard. |