Rejected at Clearinghouse Claim Secondary Identifier Description is Not to be Used
|
Rejection Message Rejected at Clearinghouse Claim Secondary Identifier Description is Not to be Used |
|
|
Rejection Details This rejection indicates an invalid authorization number or invalid character included on the authorization number is associated with the Encounter. Kareo uses the following delimiters for sending claims electronically in ANSI format: * ; and ~ Using these characters within Kareo will cause the information in the electronic claims file to move a position, resulting in a rejection. Please ensure that the above delimiters are not used in any fields in the Kareo. |
|
|
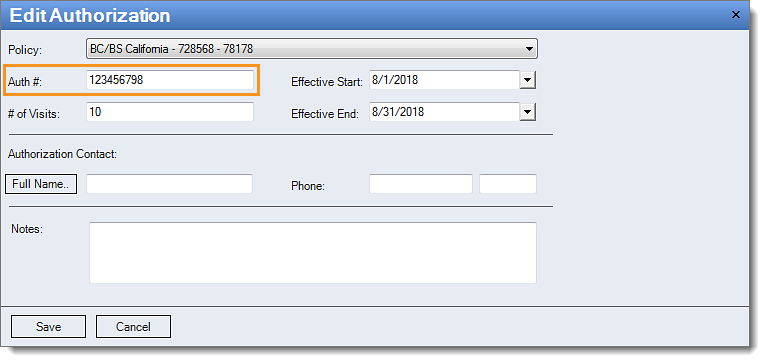
Resolution Follow the instructions below to edit the authorization number:
Then, rebill and resubmit all affected claims. |
 |